by Luminis Health
More than 38 million girls and boys under age 19 participate in organized sports each year in the United States. Among these kids, injury—from minor sprains to broken bones—is common. In fact, one in three young athletes will miss practice or games due to an injury.
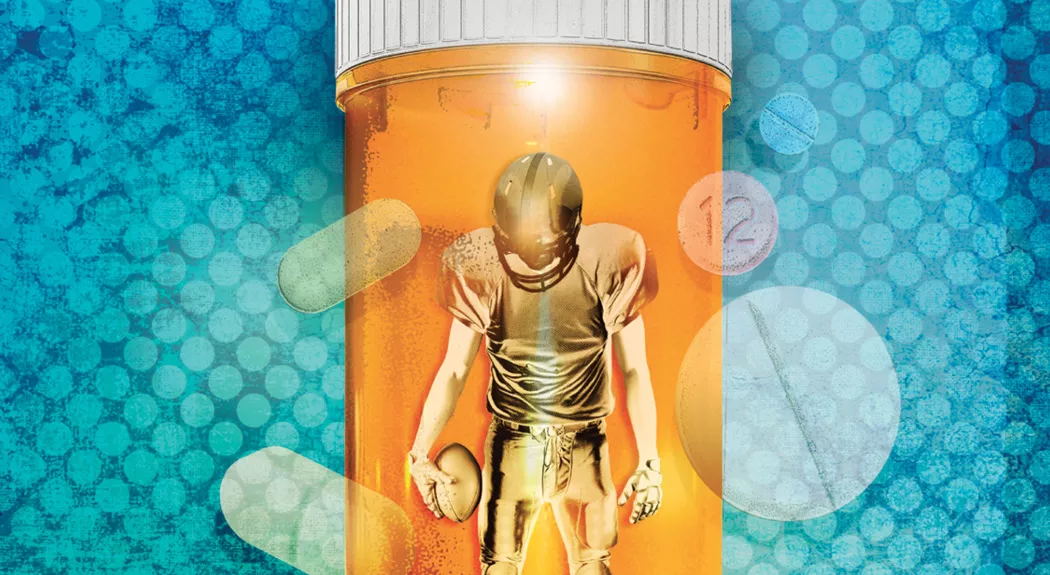
When athletes are injured, they want to get back in the game as soon as possible. The doctors treating them will determine the best way to repair their injuries and may prescribe pain medications. This is where some young people can fall into the trap of opioid addiction.
A National Crisis
Over the past two decades, addiction to opioids, which includes narcotic painkillers like Vicodin, OxyContin and Percocet—as well as heroin—has soared across the nation. In Anne Arundel County, 1,083 overdoses of heroin and other opioids were reported in 2018, according to the county Health Department. In 2015, then-Anne Arundel County Executive Steve Schuh declared a public health emergency related to heroin abuse and Maryland Governor Larry Hogan called it a statewide crisis, creating the Heroin and Opioid Emergency Task Force.
Prescription narcotic abuse is often a first step to heroin addiction. Narcotic painkillers are easy to get hooked on, and when people can’t get enough pain medication from doctors to satisfy their need, they may turn to street sources. A shocking 80 percent of all heroin users made the switch to heroin after abusing narcotic painkillers, according to the U.S. Substance Abuse and Mental Health Services Administration.
“Substance abuse disorder can happen unexpectedly. Opioid addiction can start with a simple tooth extraction or sports injury. If the pain medication is not taken as prescribed by a doctor, the tolerance level for the drug increases and you will need more of the drug to get the same effect,” says Keshia Brooks, supervisor of prevention education and family wellness at Pathways, Anne Arundel Medical Center’s (AAMC) substance abuse disorder treatment facility.
The Danger for Athletes
A study in the Journal of Adolescent Health found that boys who participate in organized sports have a higher chance of being prescribed narcotics and a higher chance of abusing them than boys who do not play sports. However, girls are more likely to be prescribed narcotics and to abuse them than boys, whether or not they play sports.
Kwasi Sharif, MD, pain management physician with AAMG Orthopedic and Sports Medicine Specialists, urges patients to consider alternative ways to manage their pain. That could include physical therapy, exercise or other medications that are not opioids.
He adds that the Centers for Disease Control and Prevention recommends non-opioid treatment for chronic pain, outside of cancer treatment, palliative care and end-of-life care.
“If parents and their student athlete decide on use of opioids, it is crucial that they use the lowest possible effective dosage to reduce risks of opioid use disorder and overdose,” Dr. Sharif says.
Programs at Pathways
Outpatient Opioid Detox Program
This program allows patients to safely withdraw from opioids over a period of three to six days, followed by ongoing professional support in recovery. For more details, visit PathwaysProgram.org or call 443-481-5400.
Family Wellness Workshop
A therapeutic and educational program for family members of adults or teens with substance use disorders brings together family members for on-site group therapy, educational sessions and personal growth. The program equips family members with communication skills, relapse prevention strategies and coping mechanisms for ongoing recovery. Full-day and weekend sessions are available. Call 410-573-5449 or visit PathwaysProgram.org for a complete schedule.
Alcohol and Drug Education Program
This program teaches adolescents about the current drug trends. It also provides training for parents on how to use Narcan, an opioid overdose reversing drug. This is a free program for Anne Arundel County teens ages 13-18 and their parents. For more details, please call 410-573-5422.
Be Cautious About Narcotics
“If a child is dealing with a sports injury and needs medication for pain, parents should first educate themselves on the various types of pain medications available and their side effects,” Keshia says.
If a physician prescribes an opioid for your child, have a conversation with the physician about the medication, she says. If possible, be the one to monitor and dispense it to your child.
“If given an opioid, ask about how long the pain medication should be taken before it can become a problem for the child,” Keshia says. “Parents should also ask what else is available besides opioids that will help with the pain. Can the child take a Tylenol or Ibuprofen?”
If you do have leftover pills from an opioid prescription, ask your pharmacy if they accept unused pills, or take them to a medication disposal box.
AAMC has two medication disposal drop boxes to dispose of unused or expired medications. The drop boxes are at MedPark Professional Pharmacy, located in the AAMC Sajak Pavilion, suite 170, 2002 Medical Parkway, Annapolis, Md., and at Arnold Professional Pharmacy, 1460 Ritchie Highway, Arnold, Md.
READ MORE: Anne Arundel Medical Center installs drop boxes for unused or expired medications
Medication Disposal
The Anne Arundel County Police Department has drop boxes at four locations for the safe disposal of unused, expired or unwanted medications. Residents can drop off medications at any time daily at the following four district stations:
- Northern District located at 939 Hammonds Lane in Baltimore, Maryland.
- Southern District located at 35 Stepneys Lane in Edgewater, Maryland.
- Eastern District located at 204 Pasadena Road in Pasadena, Maryland.
- Western District located at 8273 Telegraph Road in Odenton, Maryland.
Communication Is Key
“It is very important that parents talk to their children about opioids,” Keshia says. “Many news reports, social media, advertisements and commercials can contribute to the start of a conversation about drugs. Parents can explain to the child how some medications, especially opioids, can affect you in a negative way if not taken as prescribed and abused.”
She advises parents to discuss the signs and symptoms of substance abuse.
“Talk about what drug abuse really is: Taking medication without permission from the parents or the doctor, taking someone else’s medication, taking too much medication, or sharing medication with friends. Discuss the number of overdoses and deaths that opioids have caused right in their own community,” Keshia says. “This conversation should happen when you are teaching a child right from wrong, and should gradually increase in knowledge and understanding as the child grows up.”
Keshia also urges parents to educate themselves on what opioids are and what an overdose looks like, as well as take advantage of Narcan training opportunities.
“Sports injuries are just one of many paths young people can follow to addiction, but we have to fight this crisis on all fronts, and we don’t want parents left saying, ‘I wish I knew,’” says AAMC Chief Medical Officer Mitchell Schwartz, MD. “Beyond educating parents, we’re encouraging area primary care providers, who are often on the front lines of treating sports-related and other injuries, to know the best practices for prescribing narcotics.”
“And one of the most important roles the hospital can play in the community is to talk openly about this, removing the stigma associated with addiction so people aren’t ashamed to get help for themselves or their loved ones,” adds Dr. Schwartz. Removing the stigma is a big step toward ending the crisis.

Keshia Brooks, BSPH, MBA, is a prevention education coordinator at Pathways, AAMC’s substance abuse and mental health treatment facility. You can reach her office at 410-573-5400.
 Dr. Kwasi Sharif, MD, is a pain management physician with AAMG Orthopedic and Sports Medicine Specialists. You can reach him at 410-268-8862.
Dr. Kwasi Sharif, MD, is a pain management physician with AAMG Orthopedic and Sports Medicine Specialists. You can reach him at 410-268-8862.

Mitchell Schwartz, MD, is AAMC’s chief medical officer.
Originally published Nov. 17, 2015. Last updated Aug. 26, 2019.



